 A fungus commonly found in the dust and soil of the Mississippi and Ohio River Valley regions causes histoplasmosis. You can contract the disease by inhaling dust that carries the fungal spores. It is inhaled early in life and causes a usually symptom-free and self-limited infection throughout the body. It may affect the eye by causing small areas of inflammation and scarring of the retina, the light sensing tissue at the back of the eye. When the damage involves the central retina, distortion or blurriness of the central vision may occur.
A fungus commonly found in the dust and soil of the Mississippi and Ohio River Valley regions causes histoplasmosis. You can contract the disease by inhaling dust that carries the fungal spores. It is inhaled early in life and causes a usually symptom-free and self-limited infection throughout the body. It may affect the eye by causing small areas of inflammation and scarring of the retina, the light sensing tissue at the back of the eye. When the damage involves the central retina, distortion or blurriness of the central vision may occur.
The most important step in accurately diagnosing ocular histoplasmosis is a careful eye exam. Timely diagnosis and treatment are often successful in preventing the loss of reading vision. The retinal specialists at Bennett & Bloom Eye Centers are knowledgeable in all aspects of managing this disease. As a result, we are often able to help maintain your vision.
What is Ocular Histoplasmosis Syndrome?
The histoplasmosis fungus, which is present in soil throughout the Mississippi and Ohio River Valley regions, is inhaled early in life and causes a usually asymptomatic and self-limited infection throughout the body, including the lungs and choroid (the vascular layer lining the retina). For unknown reasons, several decades after the initial infection, the choroidal scars may develop abnormal blood vessels (macular neovascularization, CNV) which leak fluid and blood. This leakage can only be seen on a careful, dilated eye examination since the eye looks normal from the outside. Distorted central vision and loss of reading vision occur when the leakage involves the macula, that part of the retina we use for our straight-ahead reading vision. There are many causes of CNV including angioid streaks, choroidal rupture, degenerative myopia, idiopathic, and age-related macular degeneration.
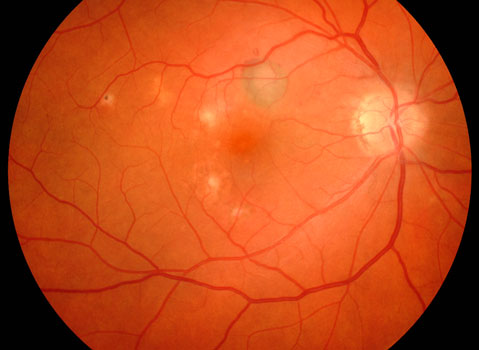
Normal macula
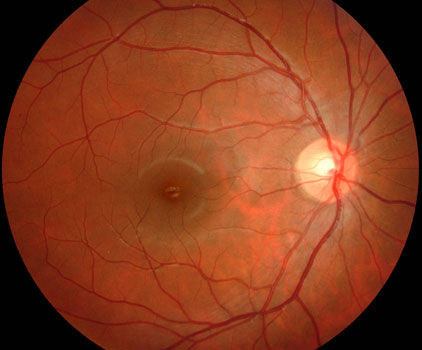
Histoplasmosis with scarring around the nerve and in the macular center
The goals of treatment are to prevent macular neovascularization from spreading into the macular center (laser photocoagulation), or limit the size of and leakage from the CNV once it reaches the macular center (photodynamic therapy, vascular endothelial growth factor inhibitors).
Who gets the Ocular Histoplasmosis Syndrome?
People who live in endemic areas who are exposed to the histoplasmosis fungus early in life are at greatest risk for developing eye problems later in life. A person with ocular histoplasmosis cannot infect other people since the organisms die soon after the initial infection. Adults who move to endemic areas, although they may get infected with the histoplasmosis fungus, do not usually develop eye disease.
What are the symptoms of the Ocular Histoplasmosis Syndrome?
People usually have no eye symptoms during the initial infection. The choroidal scars that later form also do not usually cause any symptoms. If leakage and bleeding involve the macula, symptoms such as distortion and loss of reading vision occur. Patients never go completely blind, since the part of the eye responsible for peripheral vision is not affected by this disease.

Normal vision

Ocular Histoplasmosis
Patients are often asked to check their central vision every day with an Amsler grid. This grid is a pattern that resembles a checkerboard. You should cover one eye and stare at a black dot in the center of the grid. While staring at the dot, you may notice that the straight lines in the pattern appear wavy to you. You may notice that some of the lines are missing. These may be signs of macular neovascularization.
Click here to view or download a full-sized Amsler grid for yourself.
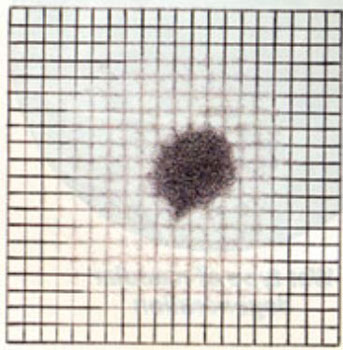
Blurry areas and black spots
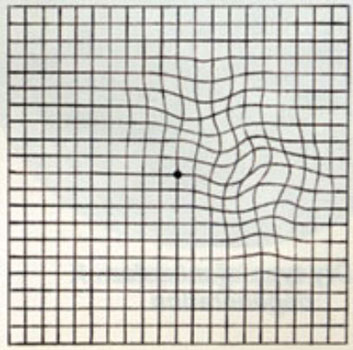
Wavy or crooked lines
How do we diagnose the Ocular Histoplasmosis Syndrome?
The most important step in accurately diagnosing the ocular histoplasmosis syndrome consists of a careful eye examination by an eye doctor familiar with all aspects of this disease. During the examination, your doctor will dilate your pupils and look for histoplasmosis scarring, leakage, and bleeding. Your doctor may need to perform an OCT scan or fluorescein angiography to better evaluate the histoplasmosis scars.
What treatments are available for ocular histoplasmosis?
Observation.
Patients with inactive histoplasmosis scarring and those who have been successfully treated are asked to look at the Amsler Grid daily for any central visual changes. If a change in the central vision or Amsler grid develops, the patient should seek prompt medical attention. A careful examination, OCT scan, and fluorescein angiogram may be needed to look for macular neovascularization that can possibly be treated.
Corticosteroids.
Steroids are potent medicines that can reduce inflammation. Some doctors will occasionally recommend steroid pills or shots for the rare patient experiencing visual symptoms from acute histoplasmosis inflammation.
Laser photocoagulation.
A laser is an instrument that produces a pure, high-intensity beam of light energy. The laser light can be focused onto the retina, selectively treating the desired area while leaving the surrounding tissues untouched. The absorbed energy heats, or photocoagulates, the retina creating a microscopic spot.
Laser surgery is performed in our office while you are awake and comfortable. The laser is used to seal the leaking vessels beneath the retina. The laser treatment usually takes less than 15 minutes to complete, and you can go home immediately following surgery. Arrangements for transportation should be made in advance since you may not be able to drive right away.
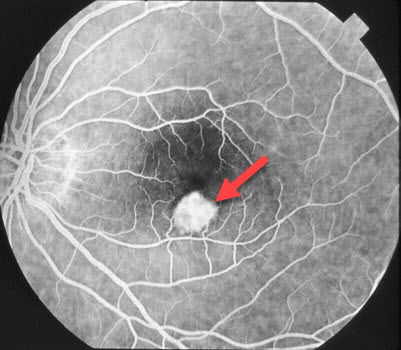
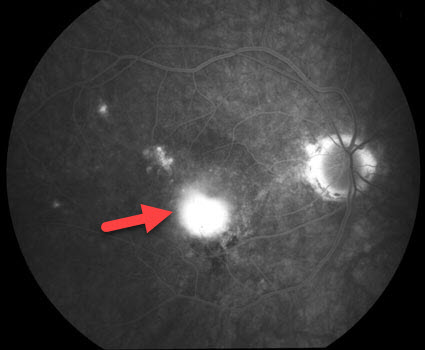
Fluorescein angiogram showing macular neovascularization (arrow)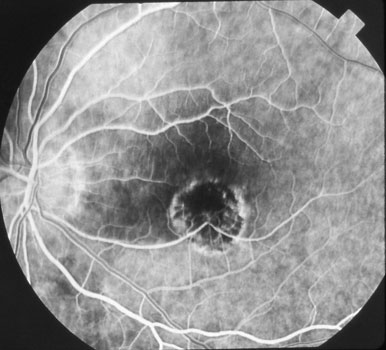
Dry laser scar following successful laser photocoagulation surgeryLaser surgery, which became available in the early 1970s, still remains an excellent treatment option for neovascularization well away from the macular center. However, for more central lesions, anti-VEGF agents and photodynamic therapy (available beginning in the early to mid-2000’s) are recommended.
Photodynamic therapy.
Laser photocoagulation surgery has traditionally been the standard treatment for patients with ocular histoplasmosis and macular neovascularization outside the macular center. When macular neovascularization is beneath the center of the macula, laser not only destroys these abnormal vessels but also permanently damages the overlying retina. Patients are thus left with a dry scar but no central vision. Photodynamic therapy, which became available in 2000, was the first modality that allowed treatment of these central lesions while minimizing retinal damage. The treatment involves injecting Verteporfin (Visudyne) intravenously, followed by painless laser treatment. Direct daylight exposure within the first 48 hours can cause a severe skin burn, so patients need to remain inside for two days following treatment. Photodynamic therapy is painless and is associated with minimal to no side effects. It usually needs to be repeated every 3 months for multiple treatments for recurrent neovascularization.
In an open-label safety study involving 26 patients with ocular histoplasmosis, visual acuity improved by an average of more than 1 line on a standard eye chart at 12 months with 28% of patients experiencing a visual acuity improvement of 3 lines or more. Visual acuity decreased by less than 3 lines of vision in 88% of patients during the same time period.
Active CNV before photodynamic therapy.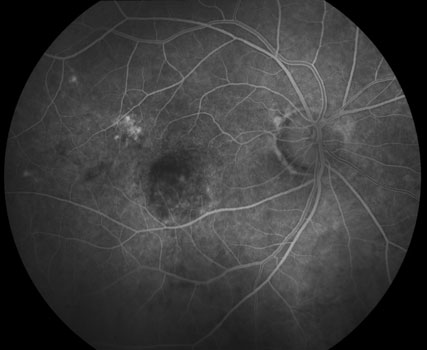
All leakage resolved following photodynamic treatmentCombining photodynamic treatment with injection of a VEGF-inhibitor or anti-inflammatory steroid medication (Kenalog) into the eye (a painless in-office procedure) appears to dramatically improve results. Patients require far fewer photodynamic treatments with combination therapy.
Vascular Endothelial Growth Factor (VEGF) Inhibitors
VEGF inhibitors (Avastin, Lucentis, and Eylea) are a new class of potent medications that prevent macular neovascularization from growing and leaking. They have been extensively studied in patients with age-related macular degeneration, and are also highly effective in ocular histoplasmosis. Click here to learn more.
Subretinal surgery.
Using advanced surgical techniques, abnormal blood vessels growing beneath the part of the eye responsible for central vision can be removed. This surgery is sometimes successful in restoring reading vision and appears mostly effective for eyes with vision worse than 20/100. Your doctor will discuss this option with you if he feels you could benefit from this procedure.
What happens if I lose my reading vision?
Except for airplane pilots, military personnel, surgeons, etc., most patients who lose reading vision in one eye usually continue their normal lifestyle and job without change. The major problem is adjusting to the initial lack of depth perception required for near vision. Eventually, patients learn to compensate for this and obtain new clues from the environment to judge close distances. Patients are usually able to thus gain back much of their lost depth perception. Patients should be able to drive a car as long as their vision in the good eye is at least 20/40 to 20/60.
Low Vision services and examination.
We may recommend that you see a specialist for a low vision examination. Magnifying lenses or other devices can be prescribed to help with reading and other central vision tasks.
For those living in the Kentuckiana and Northern Kentucky areas, the Kentucky Office for the Blind, the Cincinnati Association for the Blind and Visually Impaired, the Free Kentucky Talking Book Library Service, and the American Printing House for the Blind offer a myriad of services and resources to help those with vision loss function better and remain independent.
Radio Eye is a non-profit 24-hour radio service that broadcasts the reading of current newspapers and other everyday literature, offering greater independent living to people who are blind, visually impaired or physically handicapped. Radio Eye radio listeners hear the reading of dozens of newspapers, magazines, health materials, grocery ads and much more. The audio stream can be accessed on a special (free) Radio Eye radio, on Library Channel 20 on Lexington Insight Cable TV, in area homes and hospitals, as well as on their website.
Lighthouse Guild is a leading nonprofit vision and healthcare organization, with a long-standing heritage of addressing the needs of people who are blind or visually impaired, including those with multiple disabilities or chronic medical conditions. Through the integration of vision and healthcare services and the expansion of access through education and community outreach, their innovative and comprehensive approach helps people achieve and maintain the highest possible level of function and independence.
What are the chances of abnormal blood vessels affecting my good eye?
Patients who have no signs of abnormal blood vessels in either eye have a minimal chance of losing central vision. This risk is increased, however, if abnormal blood vessels have already affected one eye. The yearly risk for the second eye becoming involved then increases to approximately 1 in 50.
What can I do to prevent visual loss from histoplasmosis?
There is nothing that a person with histoplasmosis can do to prevent abnormal vessels from developing. The most important thing is to carefully monitor the central vision with daily vision checks (including the Amsler grid) and frequent, regular eye examinations. Any sudden change in the central vision necessitates an immediate examination by your eye doctor.
View more retina images at Retina Rocks, the world’s largest online multimedia retina image library and bibliography repository.



