What is Corneal Keratoconus & Corneal Ectasia?
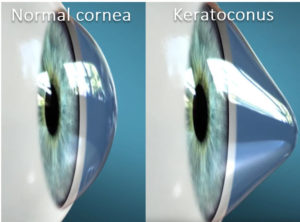
Any condition where the cornea stretches out and loses its ideal shape is considered an ectasia. Keratoconus is the most common type of corneal ectasia. When a cornea stretches out and loses its shape, it is most common for the central area of the cornea to bulge and thin out like a cone (keratoconus). Other patterns of shape changes are possible as well (pellucid marginal degeneration, keratoglobus). We generally treat all forms of ectasias the same way.
Post LASIK ectasia is a name given to any corneal thinning that occurs after LASIK surgery. Technically LASIK makes the cornea a little thinner and hence a little weaker, which slightly increases the risk of ectasia. We avoid LASIK in patients who have any suggestion of predisposed risk to ectasia or keratoconus.
What makes up a normal cornea, and what goes wrong in keratoconus?
The cornea is the strong clear tissue at the front of the eye that protects its delicate structures. The cornea also does most of the eye’s light focusing. The cornea has 3 main layers. The thin outer epithelium provides corneal sensation and is a barrier to infection. The middle structural layer, the stroma, represents the middle 85+% of the corneal thickness. It is rigid and gives the cornea its strength and shape. The thin inner endothelial layer prevents corneal swelling.
The cornea has to have the right shape to focus light well. The ideal shape is somewhat similar to a cue ball. The cornea also has to be strong to maintain this proper shape your entire life. Some corneas are not strong enough causing it to stretch-out, thin, and allow normal forces to alter its natural form. In keratoconus, the corneal shape may progress to the shape of an egg, or in severe cases, the weakened cornea can then bulge forward and sag down like a cone. Such corneas do not focus light well and distort vision.
Our corneas are weakest in youth and usually become a little stronger as we age. For this reason, keratoconus most commonly develops in the late teens to early twenties, and it can progress quickly over 10 to 20 years and then slow or even stabilize by age 40.
How common is keratoconus? What ethnic groups are most likely to get it?
About 1 in 1,000 people develop keratoconus or other ectasia. It has no known significant geographic, cultural, or social pattern.
What causes keratoconus or other ectasia?
Genetic corneal weakness, environment corneal stress, or a mixture of both. Corneal weakness is an inherited trait (genetic weakness) of various degrees. Anything that rubs and pushes on the eye (environmental stress) puts stress on the cornea. The harder the rub, the more likely a shape change will occur. People with itchy eyes and allergies are more likely to rub their eyes and develop ectasia. Extensive rubbing can even cause a sudden rupture of the inner corneal layer (Descemet’s membrane) and cause the cornea to become very painful, swollen, and blurry (acute hydrops).
What are the symptoms of keratoconus?
Keratoconus starts as a mild blurring of vision that can progress to severe distortion. Patients with keratoconus are often light sensitive and are prone to excessive tearing, especially when looking at bright lights.
What treatments can be done to help a patient with keratoconus or other ectasias to see better?
If the ectasia is mild, then glasses or soft contacts are all that is needed to see well. If the shape change is moderate, hard contacts are necessary. As the shape change gets more pronounced and irregular, special custom hard contacts are necessary. Typically, only a handful of optometrists in a given area are qualified to fit these special contacts. These contacts often save patients from needing a cornea transplant. When the shape change is severe enough, even these special contacts may not fit well and surgery may be necessary.
What are Surgical Treatments for Keratoconus?
- INTACs are small plastic rings that can be surgically inserted into a cornea to help flatten the cone to help contacts fit better.
- Corneal transplantation is typically more helpful than INTACs. There are two types of corneal transplants that we do for keratoconus: DALK or PK. Since one-third of transplants done for corneal ectasia still need a hard contact lens after surgery, transplants are not performed to get these patients out of their contacts.
How can I prevent my keratoconus/ectasia from getting worse to reduce my risk of ever needing a transplant?
Address the causes of keratoconus, which are genetic weakness and environmental stress.
- Consider a corneal strengthening procedure (Cross-linking).
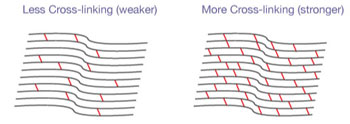 Corneal collagen cross-linking (CXL) has been used successfully in the USA and other countries for more than 15 years, and is approved by the FDA as well. Cornea crosslinking has become the international standard of care for progressive ectatic disease such as keratoconus.CXL is helpful for individuals with mild to moderate corneal ectasia that is actively progressing or at high risk for progressing. It increases the strength and rigidity of the cornea addressing its genetic weakness. CXL mostly stops further progression of the ectasia rather than reversing pre-existing corneal damage. It is not helpful for severely misshapen corneas, in pregnancy or lactating females, history of herpes corneal infection, corneal scarring, severe ocular surface disease that could likely cause poor wound healing, older individuals (since they are a low risk for disease progression), or in patients under 14 years old.
Corneal collagen cross-linking (CXL) has been used successfully in the USA and other countries for more than 15 years, and is approved by the FDA as well. Cornea crosslinking has become the international standard of care for progressive ectatic disease such as keratoconus.CXL is helpful for individuals with mild to moderate corneal ectasia that is actively progressing or at high risk for progressing. It increases the strength and rigidity of the cornea addressing its genetic weakness. CXL mostly stops further progression of the ectasia rather than reversing pre-existing corneal damage. It is not helpful for severely misshapen corneas, in pregnancy or lactating females, history of herpes corneal infection, corneal scarring, severe ocular surface disease that could likely cause poor wound healing, older individuals (since they are a low risk for disease progression), or in patients under 14 years old. In CXL, riboflavin (vitamin B2) is applied to the cornea. The cornea is then exposed to a soft blue UV light for a set period of time utilizing the Peschke CXL System. In response to this treatment, the micro-structural framework of the cornea, which is made up of collagen, develops multiple interconnections (crosslinks) that make it stronger and resistant to change shape. The eye may be uncomfortable for the first few days, with most being pain-free within a week or two. Vision is blurry for up to a month, and the glasses prescription often needs to be changed. CXL often causes a very mild reversal of the ectasia within a year.
In CXL, riboflavin (vitamin B2) is applied to the cornea. The cornea is then exposed to a soft blue UV light for a set period of time utilizing the Peschke CXL System. In response to this treatment, the micro-structural framework of the cornea, which is made up of collagen, develops multiple interconnections (crosslinks) that make it stronger and resistant to change shape. The eye may be uncomfortable for the first few days, with most being pain-free within a week or two. Vision is blurry for up to a month, and the glasses prescription often needs to be changed. CXL often causes a very mild reversal of the ectasia within a year.
- Avoid cornea weakening procedures (eye rubbing). Avoid the environmental stress of pressing on the corneas. DO NOT RUB YOUR EYES. If you or your spouse discover that you rub in your sleep (or if we simply suspect it), we will prescribe nighttime protective eye guards. If you wake up and notice that you have knocked off the eye guards, that confirms you are a nighttime rubber and that you need to tighten the strap. If you have allergies that make you want to rub your eyes, we will prescribe allergy eye drops to reduce itching. Many people have the urge to rub when removing their contacts at night. Resist this urge. It takes 10-15 minutes to go away. Some patients with severe allergies that don’t respond to drops may need to see an allergist for other treatments, including allergy shots.
Should my family members be screened?
We recommend screening other family members if you have been diagnosed with keratoconus or corneal ectasia. Diagnosed in its early stages, CXL stabilizes the disease and dramatically lessens the chance for progression.



