What is a “Boston Keratoprosthesis” or “KPro”?
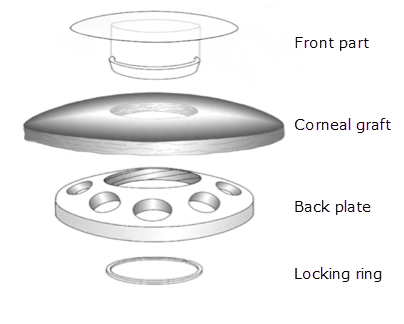
A keratoprosthesis is essentially an artificial cornea. The Boston Keratoprosthesis (KPro) is a plastic cornea implanted into the center of a transplanted donor cornea. The front lens is placed through a central hole in the corneal graft, through the back plate and then secured with a locking ring. Like one’s natural cornea, the artificial cornea focuses light. There are various focusing strengths available for the Boston Keratoprosthesis. We try to pick the strength that will minimize the need for postoperative glasses.
Who should have the KPro?
A KPro offers the best chance for improved vision when a patient cannot have a conventional full thickness corneal transplant (penetrating keratoplasty or PK). These include patients with multiple failed previous transplants, epithelial stem cell deficiency, and severe ocular surface disease.
Some patients’ immune systems aggressively reject and opacify multiple previous transplants, Even if the immune system rejects and opacifies the living outer portion of the KPro, its artificial plastic center can stay clear allowing for good vision.
In corneas that cannot maintain a healthy epithelial skin layer because of corneal epithelial stem cell deficiency, the KPro offers another option instead of a corneal epithelial stem cell transplant with subsequent PK. This option is particularly useful for patients who are not good candidates for the systemic immune suppression that is required in epithelial stem cell transplants. In cases of epithelial stem cell deficiency, a cornea cannot maintain clarity. A standard corneal transplant would not solve the problem as it would become cloudy like the original cornea. The plastic visual aspect of the KPro will not become cloudy even if epithelial stem cells are deficient.
Eyes with a significant ocular surface disease, who have a scarred, dry surface from burns or autoimmune disease, often develop cloudy sick corneas. Such patients don’t do well with a standard corneal transplant because the surface disease would cause the transplant to fail and lose its clarity. Here again, if the outer living part of the KPro opacifies, the patient can still see well through the central plastic portion. However, the living portion of the KPro is more likely to breakdown in eyes with ocular surface disease. Such breakdown carries significantly increased infection risk if not recognized quickly. An alternative surgical option for such patients would be an epithelial stem cell transplant combined with ocular surface reconstruction and/or conjunctival transplant. After the surface would heal, a regular PK may have hope of surviving.
Visual recovery with a KPro is typically faster than with a standard living cornea transplant.
What are the disadvantages of a Boston Keratoprosthesis (KPro)?
A KPro reduces one’s peripheral (side) vision. Normally we can detect objects 60 degrees towards the nose and 90 degrees toward the temple when looking straight ahead. A KPro limits the side vision to about 40 to 50 degrees in both directions.
There are more potential long term complications with a KPro than with standard cornea transplant. Some of these complications can be serious and threaten the eye. Patients are instructed to RSVP: come see us for new Redness, Sensitivity to light, Vision reduction, or Pain. For the rest of their life, any patient with a corneal transplant needs to seek immediate care if they ever develop these symptoms. Patients need to follow up on a regular basis in efforts to detect problems before they become serious. Patients typically need to be examined at least every 2 to 3 months for life.
It is difficult to measure eye pressures after KPro surgery. The center of a KPro is hard plastic which prevents accurate pressure measurements. We, therefore, have to estimate eye pressure by gently touching the top or bottom of the eye through the eyelid. High pressure in the eye damages the optic nerve (glaucoma) that can cause vision loss. Glaucoma patients typically don’t notice any symptoms until significant irreversible damage has occurred. A patient with a KPro thus has to have frequent glaucoma screening tests. If glaucoma damage is ever detected, medical and surgical treatment may be required.
As many as 10% of KPro patients may develop eye inflammation and require injections of corticosteroids around or inside their eye to help control it. These steroid injections can sometimes cause an elevation in eye pressure. This inflammation is reported to be rare or as high as 10% depending on the reports.
A membrane of cells can grow on the back of the artificial portion of the KPro in about 20 to 30% of cases. This can blur the vision. If it is significant enough, a laser is necessary to polish away the membrane. Surgical excision of the membrane is sometimes needed if it is too dense for the laser. In rare cases, the scarred membrane can be so aggressive and dense such that it recurs almost immediately after surgery to remove it. Such rare cases often respond to injection of special medication (methotrexate), but we’ve seen one case respond to nothing and require explantation.
All corneal transplants carry a risk of infection, and this risk if higher with a KPro which can occur in up to 15% of patients. The tissue around a KPro can also break down over time which could lead to extrusion of the graft and/or a serious infection inside the eye that could cause blindness or even loss of the eye. To reduce these risks, a patient with a KPro needs to take antibiotic drops for the rest of their life. Infection is more common in eyes with ocular surface disease or when patients stop taking their antibiotic drops exactly as directed. Sometimes, if we see tissue starting to thin on the edge of the KPro optic, we may want to prophylactically replace the KPro or add reinforcement tissue (corneal tissue or a conjunctival flap).
Most patients always wear a bandage contact lens to help protect the surface. Because the hard plastic of the keratoprosthesis can irritate the delicate tissue on the back of the eyelids, a soft bandage contact lens can protect the eye and keep it comfortable. This lens is not removed even when sleeping. The doctor will change it out about every 2 to 3 months.
How long do KPro’s last?
How long a KPro lasts depends on the health of the eye surface and how well the patient complies with their prescribed medication and follow-ups. There is certainly no guarantee that the KPro or the eye with a KPro in it will last a lifetime.
Do we typically perform KPro on both eyes if they need it?
Because a KPro may not last one’s entire lifetime, we often reserve KPro’s for situations when the other eye isn’t normal. If the other eye is normal and allows one to function visually, we often encourage the other eye be left as a stable “spare eye” that can be rehabilitated with a KPro at a later date if anything ever happens to the good eye. The analogy is: the damaged eye is your “spare candle that may not burn forever”… so don’t light it unless you need it.
Can a Boston Keatoprosthesis / KPro be removed?
Yes. It is possible to remove a KPro and replace it with a standard living cornea transplant. Sometimes we do this for eyes where we feared a living cornea would fail, but then we’ve encountered problems with or unique reactions to the KPro.